This page contains exclusive content for members. Log in to see full details.
Log in hereAbout the committee
The Reference Committee is a confidential Committee to the Medical Services Commission (MSC), and provides advice to the MSC on the adjudication of billing and payment disputes between physicians and the Medical Services Plan of BC (MSP). A recommendation of the Reference Committee is not binding on the Commission.
Objective
The MSC has statutory authority for the administration of the MSP and the disbursement of funds. The plan also has "medical and surgical advisers", who consider problem cases of billing and payment on behalf of the plan. When the physician involved does not agree with the advisers' opinion, such disagreements may be referred to the Reference Committee for consideration. The Reference Committee will render a written opinion and, if following the appeal process, the physician or MSP continue to disagree with the opinion, the case may be referred to the MSC for final adjudication.
Reference Committee Process
Physicians may request their case be heard by the Reference Committee if:
- There is a continuing disagreement between the physician and the MSP which exceeds 60 days from the date the physician first raises a written enquiry to the MSP with respect to an account, or;
- There is continuing dispute between the physician and the MSP over payment for services or procedures which exceeds 60 days from the date the physician first raises a written enquiry to the MSP for which no fee has been established and approved by the MSC.
How to start a Reference Committee Case:
If a physician disagrees with MSP's payment of a claim, what is the process to dispute a claim?
1. First Appeal: Resubmit your MSP billing through HIBC/ EMR by re-submitting the rejected claim. In the “note” field when resubmitting the rejected claim, indicate that you are requesting a review. Due to the EMR note character limit, longer notes can get cut off. It is strongly recommended to fax the additional information (report, consult) to MSP billing support at (250) 405-3593.
2. Recommended Second Appeal: If after first appeal, parties still do not agree, you can re-appeal the claim. If it is more than 90 days from the date of service, submission code X should be entered in correct billing field with a note asking it to be reviewed by the Medical Advisors. Please fax to MSP: A detailed letter addressed to MSP with your explanation and rationale for payment as billed, a copy of your consultation report, imaging or pictures and operative reports, and pathology, if applicable.
Physicians always have the option of submitting a case to the Reference Committee if they appealed it at least once in writing to MSP. The recommended second appeal is suggested as the Reference Committee only meets once or twice per year, which can delay payment. MSP does re-review disputed claims, especially when a detailed letter and supporting documentation is provided.
3. The last step in the appeal process: Once you’ve taken the steps above and are still not satisfied, you can choose to send your appeal via the Reference Committee. Please note this process can take time before a decision is rendered. Please fax all relevant documentation to Tara Hamilton at Doctors of BC's Department of Economics, Advocacy & Negotiations c/o the Reference Committee. The fax number is 604-638-2922 and must include all the supporting documentation, such as;
- A Letter addressed to the Reference Committee from the physician explaining their rationale for payment as billed.
- A copy of the Letter(s) from HIBC/ MSP Advisor with their rationale of why they are not paying the claim as billed.
- A copy of billings submitted and what was paid by MSP.
- A copy of the patients consultation, operative report, imaging reports or images, pathology (if applicable) related to the billing.
- A copy of your initial written enquiry and any other written correspondence sent to HIBC to support subsequent appeals.
Once all the relevant information is received:
If the physician has satisfied all the necessary requirements, a case number is assigned to the disputed claim, and a letter is sent to the physician acknowledging receipt of the necessary information. Physicians should refer to the case number when making inquiries about the claim.
For more information on the adjudication process from the BC Government, view their Billing and Payments resource page here.
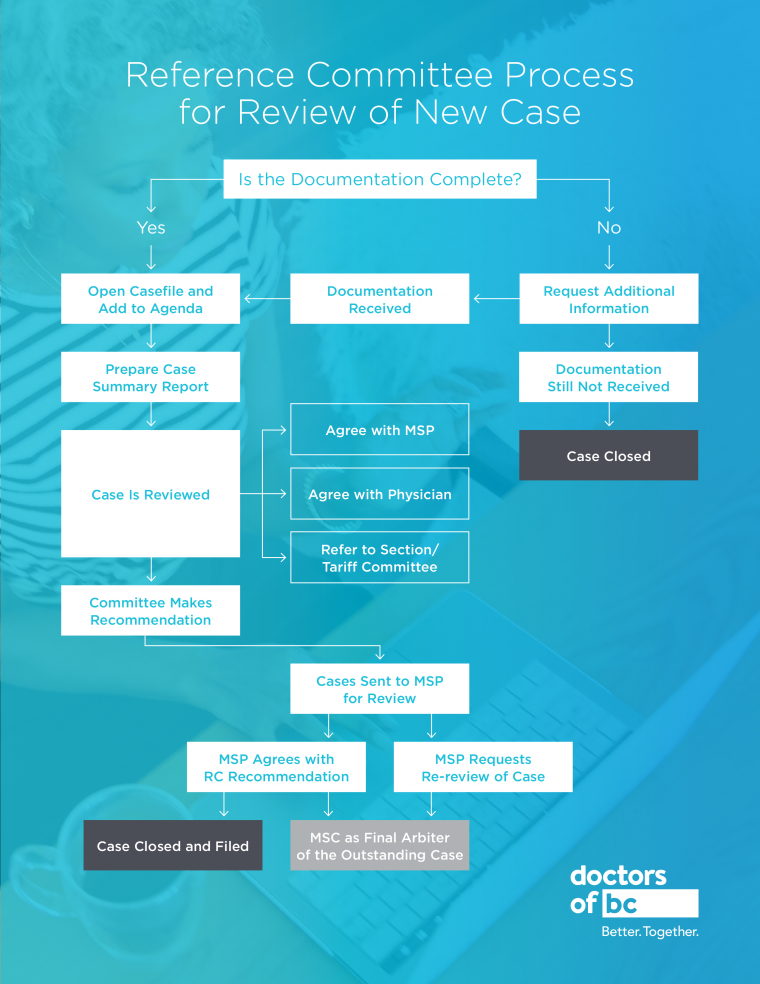
Process flow chart for receiving and reviewing reference committee cases